HIV significantly increases individuals’ atrial fibrillation risk, study suggests
A new database review of more than 17 million individuals suggests that an HIV-positive status confers a similarly significant risk for atrial fibrillation (AF) compared to other known risk factors, such as hypertension and type 2 diabetes.
In a new study, researchers from the University of California, San Francisco (UCSF; CA, USA) have found that risk of atrial fibrillation (AF) is significantly affected by HIV status. According to the National Stroke Association (CO, USA), AF affects approximately 2.2 million Americans and is a significant risk factor for stroke incidence; close to 15% of individuals who suffer strokes have underlying AF.
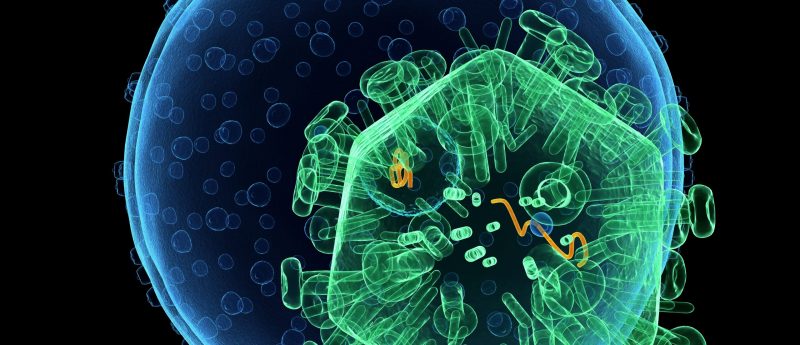
Antiretroviral therapy is one of the most effective management therapies for HIV and significantly increases the life expectancy of HIV-positive patients. Previous research has demonstrated that HIV-positive patients have increased risks of developing cardiovascular diseases and experiencing sudden cardiac death; this is thought to be due to, at least in part, antiretroviral therapy administration.
The study employed the Healthcare Cost and Utilization Project database (MD, USA) to identify 17,293,971 individuals, over the age of 21 years, who received healthcare in an outpatient surgery unit, inpatient hospital unit or emergency department, between 2005 and 2011.
18,242 study participants, equivalent to 0.11% of the total study population, had HIV.
Frequently asked questions:
Over the course of a mean 4.7-year follow-up, there were 625,167 new AF diagnoses amongst the study cohort; 1076 of these cases were in HIV-positive individuals.
When patients’ demographic characteristics, number of clinical visits and cardiovascular comorbidities were adjusted for, researchers observed HIV-positive patients to display an AF incidence rate of 18.2 per 1000 person–years, compared with 8.9 per 1000 person–years amongst HIV-negative patients.
Senior study author Gregory Marcus, a cardiologist at UCSF and associate chief of cardiology for research in the UCSF Division of Cardiology, stated: “This is the first paper demonstrating that HIV is a risk factor for AF, and the potency of that risk is similar to other well-established AF risk factors. Because AF can be asymptomatic and stroke may be the first manifestation, it’s important for caregivers to be aware of patients at heightened risk.”
Marcus concluded: “Physicians caring for HIV-infected patients should be aware of this strong relationship [between HIV and AF]. Increased awareness may help in recognizing the diagnosis and consequently result in more frequent prescription of appropriate therapies, such as anticoagulation, to reduce morbidity and mortality.”
Sources:
Sardana M, Hsue PY, Tseng ZH et al. Human Immunodeficiency Virus Infection and Incident Atrial Fibrillation. J. Am. Coll. Cardiol. 74(11); 1512–1514; (2019);
https://www.ucsf.edu/news/2019/09/415351/hiv-significantly-increases-risk-irregular-heartbeat
What is antiretroviral therapy?
Antiretrovial therapy is the recommended treatment regime for all HIV patients. Antiretroviral drugs target the virus at various stages of its life to prevent virus entry into host cells and viral replication.
What are the causes of AF?
AF manifests in an irregular, often rapid, heart rate resulting from asynchronous electrical activity of the upper heart chambers. Risk factors for the development of AF include hypertension, congenital heart disorders, coronary heart disease and hyperthyroidism, amongst others.
How may AF be managed?
AF treatments generally act to reset the heart rhythm, maintain a normal, lower heart rate and prevent blood clot formation that may otherwise lead to stroke incidence. If a patients’ AF is a result of another condition, such as hyperthyroidism, their treatment regime may include therapies that primarily manage their underlying condition.
Cardioversion may be performed to reset a patients’ heart rhythm: this can involve surgery or phamacotherapy administration. Beta blockers or cardiac glycosides may be prescribed to maintain a low heart rate. Anticoagulant drugs may be used to prevent blood clot formation.
